Introduction to Atherosclerosis
Atherosclerosis is a term that often comes up in discussions about heart health, but do you really know what it entails? At its core, atherosclerosis is the buildup of fatty deposits, cholesterol, and other substances in and on the artery walls. This buildup can lead to serious problems, including heart attacks, strokes, and even death. Understanding atherosclerosis, especially in its peripheral form, is crucial for preventing and managing this silent threat.
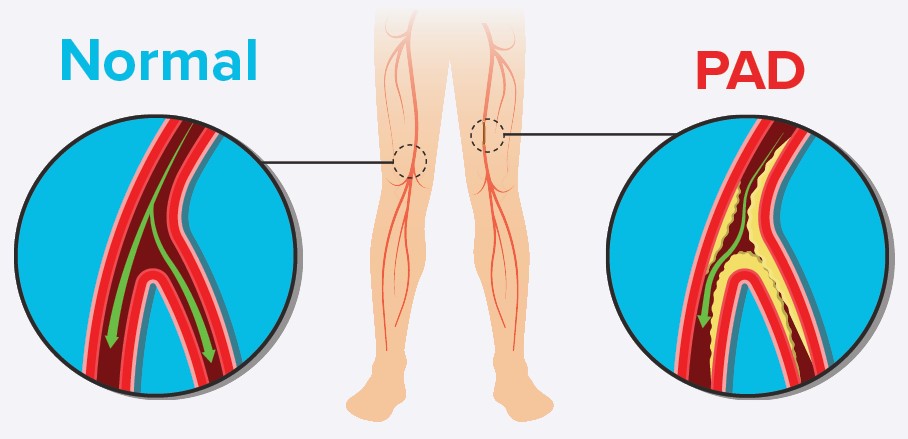
What is Peripheral Atherosclerosis?
Peripheral atherosclerosis, or peripheral artery disease (PAD), occurs when atherosclerosis affects the arteries that supply blood to the limbs, usually the legs. Unlike coronary atherosclerosis, which affects the arteries leading to the heart, peripheral atherosclerosis can cause pain and mobility issues, severely impacting quality of life.
Causes and Risk Factors
Genetic Predisposition
Genetics play a significant role in the development of peripheral atherosclerosis. If you have a family history of heart disease or atherosclerosis, your risk is higher.
Lifestyle Choices
Unhealthy lifestyle choices, such as a poor diet high in saturated fats and cholesterol, lack of exercise, smoking, and excessive alcohol consumption, can increase the risk of developing peripheral atherosclerosis.
Other Medical Conditions
Certain medical conditions, including diabetes, hypertension, and high cholesterol, also contribute to the risk of peripheral atherosclerosis.
Symptoms of Peripheral Atherosclerosis
Early Signs
Early symptoms of peripheral atherosclerosis can be subtle, often mistaken for regular aging or other less severe conditions. These may include intermittent claudication, which is pain or cramping in the legs triggered by physical activity and relieved by rest.
Advanced Symptoms
As the condition progresses, symptoms become more severe. These can include persistent leg pain, numbness, weakness, and even sores or ulcers on the feet or legs that do not heal properly.
Diagnosis of Peripheral Atherosclerosis
Physical Examination
A physical examination can reveal signs of peripheral atherosclerosis, such as weak or absent pulses in the legs, decreased blood pressure in the affected limb, and sores or wounds that heal poorly.
Diagnostic Tests and Imaging
To confirm the diagnosis, doctors may use various tests, including ankle-brachial index (ABI), ultrasound, magnetic resonance angiography (MRA), and computed tomography angiography (CTA).
Impact of Peripheral Atherosclerosis on Health
Complications and Related Health Issues
Peripheral atherosclerosis can lead to severe complications, including critical limb ischemia, where blood flow to the limbs is severely restricted, potentially leading to tissue death and amputation.
Quality of Life
The pain and mobility issues associated with peripheral atherosclerosis can drastically reduce a person’s quality of life, making daily activities challenging.
Prevention Strategies
Healthy Diet
Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins while reducing intake of saturated fats, trans fats, and cholesterol can help prevent peripheral atherosclerosis.
Regular Exercise
Engaging in regular physical activity, such as walking, cycling, or swimming, can improve blood flow and reduce the risk of atherosclerosis.
Avoiding Tobacco and Excessive Alcohol
Smoking cessation and limiting alcohol intake are crucial steps in preventing peripheral atherosclerosis.
Treatment Options
Medications
Several medications can help manage peripheral atherosclerosis, including statins to lower cholesterol, antiplatelets to prevent blood clots, and medications to control blood pressure and diabetes.
Surgical Interventions
In severe cases, surgical interventions such as angioplasty, where a balloon is used to open up the artery, or bypass surgery, where a graft is used to bypass the blocked artery, may be necessary.
Lifestyle Changes
Making significant lifestyle changes, such as improving diet, increasing physical activity, and managing stress, can significantly impact the management of peripheral atherosclerosis.
Medications for Peripheral Atherosclerosis
Statins
Statins help lower cholesterol levels in the blood, reducing the buildup of plaques in the arteries.
Antiplatelets
Antiplatelet medications, such as aspirin, help prevent blood clots from forming, which can obstruct narrowed arteries.
Other Medications
Other medications may include those that manage hypertension and diabetes, which are critical in controlling the overall risk of atherosclerosis.
Surgical and Non-Surgical Interventions
Angioplasty
Angioplasty is a minimally invasive procedure that involves inflating a balloon inside the artery to widen it and improve blood flow.
Bypass Surgery
Bypass surgery involves creating a new pathway for blood flow around the blocked artery using a graft from another part of the body.
Minimally Invasive Procedures
Other minimally invasive procedures, such as stenting, involve placing a small wire mesh tube inside the artery to keep it open.
Lifestyle Modifications
Diet and Nutrition
Eating a balanced diet that is low in saturated fats, cholesterol, and sodium can help manage and prevent peripheral atherosclerosis.
Physical Activity
Regular physical activity improves circulation and overall cardiovascular health, which is crucial for managing peripheral atherosclerosis.
Stress Management
Practicing stress management techniques, such as yoga, meditation, and deep breathing exercises, can help lower blood pressure and improve heart health.
Living with Peripheral Atherosclerosis
Daily Management Tips
Managing peripheral atherosclerosis involves regular monitoring of symptoms, adhering to treatment plans, and maintaining a healthy lifestyle.
Support Systems and Resources
Joining support groups and utilizing resources such as counseling and educational materials can provide emotional support and practical advice for managing the condition.
Research and Future Directions
Current Research
Ongoing research aims to better understand the mechanisms behind peripheral atherosclerosis and develop more effective treatments.
Future Innovations and Treatments
Future innovations may include advanced medications, improved surgical techniques, and new technologies for early detection and management.
Myths and Misconceptions
Common Misunderstandings
There are many myths about peripheral atherosclerosis, such as it being solely a problem for the elderly or that it cannot be managed effectively.
Facts vs. Myths
Dispelling these myths is essential to encourage proactive management and treatment of the condition.
Conclusion
Peripheral atherosclerosis is a serious condition that requires attention and proactive management. By understanding the causes, symptoms, and treatment options, individuals can take steps to prevent and manage this disease effectively. Healthy lifestyle choices, regular medical check-ups, and adherence to treatment plans can significantly improve outcomes and quality of life.
FAQs
What is the difference between peripheral and coronary atherosclerosis?
Peripheral atherosclerosis affects the arteries that supply blood to the limbs, while coronary atherosclerosis affects the arteries that supply blood to the heart.
How can I reduce my risk of developing peripheral atherosclerosis?
You can reduce your risk by adopting a healthy diet, engaging in regular physical activity, avoiding tobacco, and managing medical conditions such as diabetes and hypertension.
What are the common symptoms of peripheral atherosclerosis?
Common symptoms include leg pain or cramping during physical activity, numbness, weakness, and sores or ulcers on the feet or legs that do not heal properly.
Are there effective treatments available for peripheral atherosclerosis?
Yes, treatments include medications, surgical interventions, and lifestyle changes aimed at improving blood flow and managing symptoms.
How can lifestyle changes impact the management of peripheral atherosclerosis?
Lifestyle changes, such as a healthy diet, regular exercise, and stress management, can significantly improve blood flow, reduce symptoms, and prevent further progression of the disease.