
Karla Renée was 18 weeks into her pregnancy when she and her husband Sam learned that the fetus had a serious genetic anomaly that could lead to severe physical and mental disabilities. They were faced with an enormous and pressing decision. In North Carolina, where they live, the current law forbids abortion after 20 weeks gestational age.
Max Posner/NPR
hide caption
toggle caption
Max Posner/NPR

Karla Renée was 18 weeks into her pregnancy when she and her husband Sam learned that the fetus had a serious genetic anomaly that could lead to severe physical and mental disabilities. They were faced with an enormous and pressing decision. In North Carolina, where they live, the current law forbids abortion after 20 weeks gestational age.
Max Posner/NPR
In April, Karla Renée got a surprise positive on a pregnancy test. She and her husband Sam had tried unsuccessfully to get pregnant before and had expected they’d need fertility treatments.
“For it to just happen naturally felt like a miracle,” she says. “We were ecstatic.”
By the time she found a doctor in her insurance network near where she lived outside of Raleigh, N.C., and got in for her first appointment, she was eight weeks pregnant.
“The doctor noted that since I’ll be 35 when the baby was due, I should take a screening test for genetic anomalies,” she says. “We agreed to do the test and we scheduled our next appointment for a month out.”
For those few weeks, they were just “blissfully pregnant,” she says.
At the 12-week appointment, the doctor noticed something called increased nuchal translucency in the ultrasound. This happens when extra fluid accumulates behind the neck of a fetus. “We’d never heard [of] that before,” says Karla. “She explained that lots of babies have this and they can recover on their own, but it could be an indication of something more serious.”
The first genetic screening results, from blood tests, came in — they were negative for several common genetic conditions. That test also told them they were having a girl. “We felt relief and we felt hope, and we started to call her Amber,” Karla says.

Their ob-gyn recommended a second, more comprehensive genetic test – amniocentesis – to see if there was a cause for the fluid accumulation she’d observed on the ultrasound. It’s often done when there’s a family history of certain genetic conditions, or the patient is over 35, or the doctor wants to follow up on an unusual result from a previous test.
That test involved waiting several more weeks until cells could be gathered, cultured and analyzed.
The results, which Karla finally got at week 18 of her pregnancy, showed their fetus had monosomy 18p – a condition in which all or part of the short arm of chromosome 18 is missing. Their doctors told them their daughter would likely have severe intellectual and physical disabilities, and could potentially need medical interventions as soon as she was born.
Karla and Sam were in shock but they didn’t have much time to process. They needed to make an enormous decision: whether to continue or terminate their pregnancy.
They received the test results on June 27 – three days after Roe v. Wade was overturned. North Carolina had a 20-week abortion ban on the books that was blocked by the courts. That law was expected to go into effect imminently, so Karla said that hospitals were “taking no chances with legal liability.” She was told if she decided to terminate the pregnancy, she needed to get in before 20 weeks, or she would have to travel out of state.
North Carolina also has a 72-hour waiting period for abortions, meaning if they did decide to terminate, they would have to wait at least three days before getting the procedure.
They only had a few days to determine the course of the rest of their lives.
The situation: 18 weeks into her pregnancy, Karla Renée learned the baby she was carrying had a serious genetic anomaly that could lead to severe physical and mental disabilities, miscarriage or stillbirth.
The state law: North Carolina’s current law forbids abortion after 20 weeks gestational age. The law was passed in 1973 – it had been blocked by a judge in 2019 because Roe v. Wade protected the right to abortion until viability, which is generally considered to be about 24 weeks gestational age. But on the very day of the Supreme Court ruling in June, the leaders of the state senate and house – both Republicans – sent a letter to the state attorney general requesting that he take steps to put the 20-week ban into effect. Ultimately, the judge lifted his injunction and the law went into effect on Aug. 17 this year.
The only case in which abortion is legal in North Carolina after the 20-week limit is if continuing the pregnancy “would threaten the life or gravely impair the health of the woman.” There is no exception for rape and incest, or for fetal anomalies.
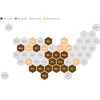
North Carolina is one of at least a dozen states that set a gestational limit on abortion earlier than the Roe-era limit of fetal viability. The cutoffs in these laws range from 6 weeks up to 22 weeks. Few states have exceptions for fetal anomalies.

We want to hear from you: NPR is reporting on personal stories of lives affected by abortion restrictions in the post-Roe era. Do you have story about how your state’s abortion laws changed your life? Share your story.
What’s at stake: Serious problems with fetal development often aren’t identified until around the midpoint of pregnancy, says Dr. Neeta Vora, a professor of maternal-fetal medicine at UNC-Chapel Hill and director of reproductive genetics, who was not involved in Karla Renée’s care. In states with gestational age limits, that knowledge can come too late, or arrive extremely close to the legal cut-off, making parents have to rush to decide what they want to do.
A noninvasive screening blood test can find relatively common genetic conditions – including Down syndrome, trisomy 13, and trisomy 18 – as early as 10 weeks into a pregnancy. If there’s a reason to suspect a genetic condition – for instance if there’s a family history or something noticed on an ultrasound or a patient is older than 35, doctors may use a diagnostic test to create a complete set of chromosomes to diagnose problems that the screening test may miss.
The first diagnostic test available, which is done by sampling the placenta, is called chorionic villus sampling. It’s available as early as 10 weeks. However, amniocentesis, the other diagnostic option which samples the amniotic fluid, isn’t recommended until after 15 weeks of pregnancy, and the results can take several weeks to come back. That puts many people in the same position as the Renées – finding out around 18 weeks that their fetus has a serious genetic condition, including ones that are fatal.
There are also developmental issues that aren’t apparent until even later in pregnancy, Vora explains. An “anatomy scan” ultrasound is usually done around 20 weeks, and can find abnormalities of the heart, spinal cord, brain, and other organs.
She says often patients come to that ultrasound appointment excited, with no idea there’s anything wrong. “Unfortunately, we do have to sort of drop bombs on patients who come in – sometimes they just think everything’s normal, they think they’re going to find out the gender, and then there’s an anomaly,” Vora says.
It can take time for people to process the information. As much as they can, doctors will try to help patients understand what is wrong and what that means, but often there is imperfect information.
There are conditions where the prognosis can be good – depending on severity of symptoms and the support available to them, patients can thrive, she says. More serious conditions can require extensive medical interventions throughout a person’s life, and that care comes with financial and emotional costs to the family.
Then there are “life limiting” conditions – meaning the infant might be stillborn or die within a few hours or days of birth. If parents opt to continue a pregnancy in these cases, Vora tells them about palliative care options to make their newborn’s short life as comfortable as possible.
Still others are considered “gray diagnoses,” where it’s very hard to know the severity or prognosis for each case in utero. Parents who receive any fetal diagnosis face a lot of uncertainty about exactly how the disorder will manifest in their child and what it will mean for the family.
When parents live in a state with a gestational limit on abortion, they may not have much time to decide what to do, Vora says. “Now, artificially, it is becoming a fast process,” she says. “That’s very difficult for people.”
The impact: The days after Sam and Karla Renée received the diagnosis were “a frenzy of research” into monosomy 18p, Karla says.
There is not a lot of information available about this particular disorder – Karla says her ob-gyn had never heard of it. According to the National Organization for Rare Disorders, the condition is characterized by head and face malformations, and other physical and mental disabilities that vary depending on how much of the chromosome is missing. In the most severe cases, the fetus can have brain malformation and die in infancy.

Karla kept a pair of hospital socks that her all-female care team had put on her following the abortion. To her, the socks symbolized the care that the team had given her throughout the procedure.
Max Posner/NPR
hide caption
toggle caption
Max Posner/NPR

Karla kept a pair of hospital socks that her all-female care team had put on her following the abortion. To her, the socks symbolized the care that the team had given her throughout the procedure.
Max Posner/NPR
Karla and Sam Renée were told that theirs was a severe case. “She really couldn’t have had more of that [chromosomal] arm deleted – they told us they could barely find any of it at all,” Karla says. Their doctors and genetic counselors emphasized that the couple should expect severe symptoms, but weren’t able to say exactly what they would be.
“We didn’t know if she could use her legs – we never felt her kick, not even once,” Karla says. “She could have needed surgery on her organs. There [were] indications that she might have needed surgery on her jaw just to be able to eat. We didn’t know if she’d be able to speak.”
A follow-up ultrasound had also shown the increased nuchal translucency had developed into a cystic hygroma, a type of cyst at the neck that can increase the risk of miscarriage or stillbirth, along with with heart and skeletal problems.
If she did survive, they wondered what kind of life she would have. “I saw some people on YouTube had kind of a similar disorder – something adjacent,” Sam says. “I did find one person with a mild case, but it still left so much uncertainty.”
They looked into social services in their area but weren’t confident they would be able to get what they needed. “If we couldn’t even be assured that there were support services for her or for families like ours, what’s going to happen when she gets older and when we’re gone?” Karla says.
“When you combine all of those physical and mental and emotional pieces together, I couldn’t ask my daughter to walk that path – it’s too much,” she says. “I felt it would be selfish to ask her to stay and to go through all that, just for us to be parents.”
Karla recalls “thrashing and flailing in the face of this decision we didn’t want to have to make. We wanted to go buy onesies and make a nursery, but instead, we had to think through this.”
After several sleepless nights, Karla and Sam decided to end their pregnancy.
Making that decision is “an immense responsibility that I feel is rightfully mine,” Karla says. “I’m the one who has to live with this. I’m the one who has to make the call.”
Although the North Carolina law banning abortion after 20 weeks was still in legal limbo, the hospital scrambled to get her in — and were able to schedule the abortion at 19 weeks, 6 days.
The policy debate: In North Carolina, the gestational age limit may not be 20 weeks for much longer. The North Carolina legislature is Republican-controlled and the senate leader, Phil Berger, has said he supports a 12- to 15-week ban. The speaker of the house, Tim Moore, has said he supports a ban closer to six weeks. (Neither Moore or Berger granted NPR’s request for an interview on abortion limits for this story.)
At the federal level, Lindsey Graham, the senior Republican senator from neighboring South Carolina, has drafted a 15-week national ban. At that stage of pregnancy, some cases of serious fetal anomalies could not be detected yet in testing.
And there are very few exceptions in state abortion laws for fetal anomalies, even lethal ones.
All states that have near-total or six-week abortion bans include an exception for when the pregnant person’s life is in danger, according to Elizabeth Nash, a state policy analyst at the Guttmacher Institute. A few states allow exceptions for rape or incest. But “the least common exception” is for fetal anomalies, explains Nash. “If you look back over the past several decades, an exception for [fetal] anomaly has been very uncommon.”
In fact, in recent years, some states have moved in the other direction, passing laws banning abortion because of a diagnosis of disability or genetic condition. North Carolina legislators passed such a law last year but it was vetoed by the Democratic governor.
But now? A version of that bill is back in the current legislative session. It states that “human dignity includes the inherent right not to suffer discrimination on the basis of innate characteristics, such as a human being’s race, sex, or genetic characteristics, including any genetic abnormalities.”
In other words, abortion for these reasons is framed as discrimination against the fetus.
Some disability rights activists push back on framing the issue this way, and support people making their own reproductive decisions, not the state. “In the disability community, we very strongly believe that bodily autonomy is sacred,” says Rebecca Cokley, a program officer at the Ford Foundation’s Disability Rights program.
“While it may be difficult and heartbreaking for some of us to live with the reality that we have friends or loved ones that may abort a fetus because they’re just like us,” Cokley says, “at the end of the day, the right to bodily autonomy and the need to preserve that right is of greater importance, because we spend our whole lives being told we don’t have rights to our bodies.”
She adds that people with disabilities don’t like their cause to be used in political arguments. “[Our] lives are not meant to be pieces on a chessboard for the punditry to move around.”

Karla and Sam had a memorial plaque placed in a fern garden outside their home. They don’t plan to try to get pregnant again anytime soon.
Max Posner/NPR
hide caption
toggle caption
Max Posner/NPR

Karla and Sam had a memorial plaque placed in a fern garden outside their home. They don’t plan to try to get pregnant again anytime soon.
Max Posner/NPR
The parents’ perspective: When Karla woke up after her abortion procedure, she found her feet had been covered with fuzzy gray socks. She felt moved that someone would show that kind of care, while she went through surgery to end her deeply wanted pregnancy.
She kept the socks. She also kept the ultrasound images, putting them and other mementos into a scrapbook. In the woods behind their house, the couple placed a stone marker near a circle of ferns. They can see the memorial from their backdoor.
Karla has found support in an online group for people who’ve been through the same thing. She and Sam are grateful for the understanding and kindness of colleagues – including the person who dropped off soup at their door. They don’t plan to try to get pregnant again anytime soon.
Meanwhile, on the news, people are debating abortion limits at this many weeks or that many weeks in a detached, abstract way. “It’s surreal watching people fight about whether I should have had the right,” Karla says.
She thinks these conversations about morality and laws and what states should do are important, and she’s started to jump into them a bit, including on Reddit.
People who’ve gone through what’s called a “termination for medical reasons” aren’t usually part of the conversation, she says. “I don’t think it’s because we don’t want to be considered or included, it’s that this is such a deep and private pain, and it’s hard to talk about.”
She does want to be part of the conversation, and that’s why she’s sharing her story about what it’s really like to receive a serious fetal diagnosis and make the difficult decision to terminate – in a country where many state laws are making that option harder to secure.
Days & Weeks is NPR’s series telling personal stories of lives affected by abortion restrictions in the post-Roe era. Do you have story about how your state’s abortion laws have changed your life? Share your story.


