The federal system meant to stop health care business owners and executives from repeatedly bilking government health programs fails to do so, a KHN investigation has found.
That means people are once again tapping into Medicaid, Medicare, and other taxpayer-funded federal health programs after being legally banned because of fraudulent or illegal behavior.
In large part that’s because the government relies on those who are banned to self-report their infractions or criminal histories on federal and state applications when they move into new jobs or launch companies that access federal health care dollars.
The Office of Inspector General for the U.S. Department of Health and Human Services keeps a public list of those it has barred from receiving any payment from its programs — it reported excluding more than 14,000 individuals and entities since January 2017 — but it does little to track or police the future endeavors of those it has excluded.
The government explains that such bans apply to “the excluded person” or “anyone who employs or contracts with” them. Further, “the exclusion applies regardless of who submits the claims and applies to all administrative and management services furnished by the excluded person,” according to the OIG.
Federal overseers largely count on employers to check their hires and identify those excluded. Big hospital systems and clinics typically employ compliance staff or hire contractors who routinely vet their workers against the federal list to avoid fines.
However, those who own or operate health care businesses are typically not subject to such oversight, KHN found. And people can sidestep detection by leaving their names off key documents or using aliases.
“If you intend to violate your exclusion, the exclusion list is not an effective deterrent,” said David Blank, a partner at Arnall Golden Gregory who previously was senior counsel at the OIG. “There are too many workarounds.”
KHN examined a sample of 300 health care business owners and executives who are among more than 1,600 on OIG’s exclusion list since January 2017. Journalists reviewed court and property records, social media, and other publicly available documents. Those excluded had owned or operated home health care agencies, medical equipment companies, mental health facilities, and more. They’d submitted false claims, received kickbacks for referrals, billed for care that was not provided, and harmed patients who were poor and old, in some cases by stealing their medication or by selling unneeded devices to unsuspecting Medicare enrollees. One owner of an elder care home was excluded after he pleaded guilty to sexual assault.
Among those sampled, KHN found:
- Eight people appeared to be serving or served in roles that could violate their bans;
- Six transferred control of a business to family or household members;
- Nine had previous, unrelated felony or fraud convictions, and went on to defraud the health care system;
- And seven were repeat violators, some of whom raked in tens of millions of federal health care dollars before getting caught by officials after a prior exclusion.
The exclusions list, according to Blank and other experts, is meant to make a person radioactive — easily identified as someone who cannot be trusted to handle public health care dollars.
But for business owners and executives, the system is devoid of oversight and rife with legal gray areas.
One man, Kenneth Greenlinger, pleaded guilty in 2016 to submitting “false and fraudulent” claims for medical equipment his California company, Valley Home Medical Supply, never sent to customers that totaled more than $1.4 million to Medicare and other government health care programs, according to his plea agreement. He was sentenced to eight months in federal prison and ordered to pay restitution of more than $1 million, according to court records. His company paid more than $565,000 to resolve allegations of false claims, according to the Justice Department website.
Greenlinger was handed a 15-year exclusion from Medicare, Medicaid, and any other federal health care program, starting in 2018, according to the OIG.
But this October, Greenlinger announced a health care business with government contracts for sale. Twice on LinkedIn, Greenlinger announced: “I have a DME [durable medical equipment] company in Southern California. We are contracted with most Medicare and Medi-Cal advantage plans as well as Aging in Place payers. I would like to sell,” adding a Gmail address.
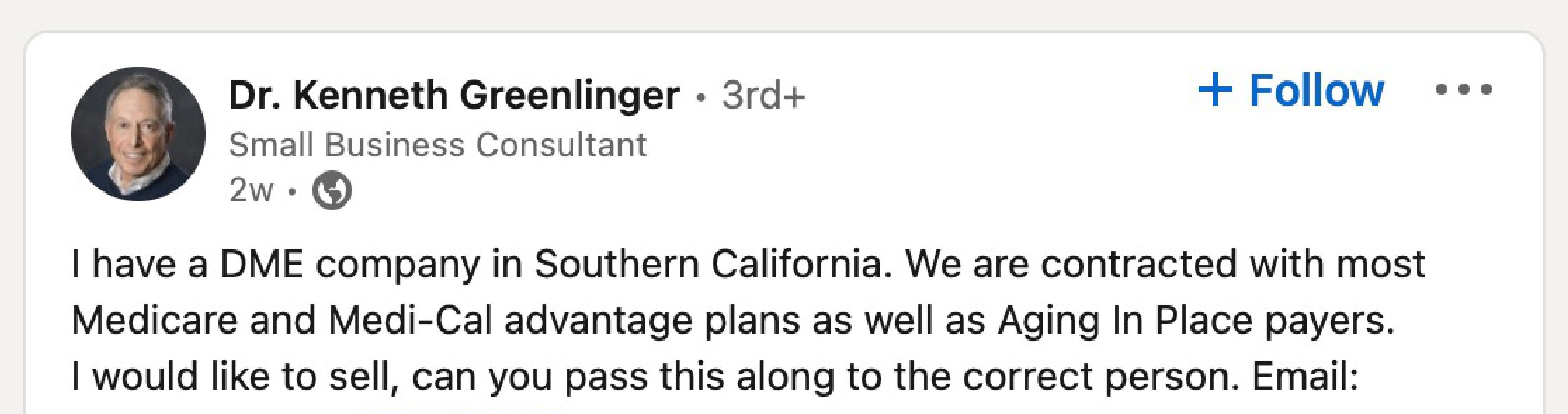
Reached by phone, Greenlinger declined to comment on his case. About the LinkedIn post, he said: “I am not affiliated directly with the company. I do consulting for medical equipment companies — that was what that was, written representing my consulting business.”
His wife, Helene, who previously worked for Valley Home Medical Supply, is now its CEO, according to LinkedIn and documentation from the California Secretary of State office. Although Helene has a LinkedIn account, she told KHN in a telephone interview that her husband had posted on her behalf. But Kenneth posted on and commented from his LinkedIn page — not his wife’s.
At Valley Home Medical Supply, a person who answered the phone last month said he’d see whether Kenneth Greenlinger was available. Another company representative got on the line, saying “he’s not usually in the office.”
Helene Greenlinger said her husband may come by “once in a while” but “doesn’t work here.”
She said her husband doesn’t do any medical work: “He’s banned from it. We don’t fool around with the government.”
“I’m running this company now,” she said. “We have a Medicare and Medi-Cal number and knew everything was fine here, so let us continue.”
No Active Enforcement
Federal regulators do not proactively search for repeat violators based on the exclusion list, said Gabriel Imperato, a managing partner with Nelson Mullins in Florida and former deputy general counsel with HHS’ Office of the General Counsel in Dallas.
He said that for decades he has seen a “steady phenomenon” of people violating their exclusions. “They go right back to the well,” Imperato said.
That oversight gap played out during the past two years in two small Missouri towns.
Donald R. Peterson co-founded Noble Health Corp., a private equity-backed company that bought two rural Missouri hospitals, just months after he’d agreed in August 2019 to a five-year exclusion that “precludes him from making any claim to funds allocated by federal health care programs for services — including administrative and management services — ordered, prescribed, or furnished by Mr. Peterson,” said Jeff Morris, an attorney representing Peterson, in a March letter to KHN. The prohibition, Morris said, also “applies to entities or individuals who contract with Mr. Peterson.”
That case involved a company Peterson created called IVXpress, now operating as IVX Health with infusion centers in multiple states. Peterson left the company in 2018, according to his LinkedIn, after the settlement with the government showed a whistleblower accused him of altering claims, submitting false receipts for drugs, and paying a doctor kickbacks. He settled the resulting federal charges without admitting wrongdoing. His settlement agreement provides that if he violates the exclusion, he could face “criminal prosecution” and “civil monetary penalties.”
In January 2020, Peterson was listed in a state registration document as one of two Noble Health directors. He was also listed as the company’s secretary, vice president, and assistant treasurer. Four months later, in April 2020, Peterson’s name appears on a purchasing receipt obtained under the Freedom of Information Act. In addition to Medicare and Medicaid funds, Noble’s hospitals had received nearly $20 million in federal covid relief money.
A social media account with a photo that appears to show Peterson announced the launch of Noble Health in February 2020. Peterson identified himself on Twitter as executive chairman of the company.

It appears federal regulators who oversee exclusions did not review or approve his role, even though information about it was publicly available.
Peterson, whose name does not appear on the hospitals’ Medicare applications, said by email that his involvement in Noble didn’t violate his exclusion in his reading of the law.
He said he owned only 3{7b6cc35713332e03d34197859d8d439e4802eb556451407ffda280a51e3c41ac} of the company, citing OIG guidance — federal regulators may exclude companies if someone who is banned has ownership of 5{7b6cc35713332e03d34197859d8d439e4802eb556451407ffda280a51e3c41ac} or more of them — and he did not have a hand in operations. Peterson said he worked for the corporation, and the hospitals “did not employ me, did not pay me, did not report to me, did not receive instructions or advice from me,” he wrote in a November email.
A 2013 OIG advisory states that “an excluded individual may not serve in an executive or leadership role” and “may not provide other types of administrative and management services … unless wholly unrelated to federal health care programs.”
Peterson said his activities were apart from the business of the hospitals.
“My job was to advise Noble’s management on the acquisition and due diligence matters on hospitals and other entities it might consider acquiring. … That is all,” Peterson wrote. “I have expert legal guidance on my role at Noble and am comfortable that nothing in my settlement agreement has been violated on any level.”
For the two hospitals, Noble’s ownership ended badly: The Department of Labor opened one of two investigations into Noble this March in response to complaints from employees. Both Noble-owned hospitals suspended services. Most employees were furloughed and then lost their jobs.
Peterson said he left the company in August 2021. That’s the same month state regulators cited one hospital for deficiencies that put patients “at risk for their health and safety.”
If federal officials determine Peterson’s involvement with Noble violated his exclusion, they could seek to claw back Medicaid and Medicare payments the company benefited from during his tenure, according to OIG records.
Enforcement in a Gray Zone
Dennis Pangindian, an attorney with the firm Paul Hastings who had prosecuted Peterson while working for the OIG, said the agency has limited resources. “There are so many people on the exclusions list that to proactively monitor them is fairly difficult.”
He said whistleblowers or journalists’ reports often alert regulators to possible violations. KHN found eight people who appeared to be serving or served in roles that could violate their bans.
OIG spokesperson Melissa Rumley explained that “exclusion is not a punitive sanction but rather a remedial action intended to protect the programs and beneficiaries from bad actors.”
But the government relies on people to self-report that they are banned when applying for permission to file claims that access federal health care dollars through the Centers for Medicare & Medicaid Services.
While federal officials are aware of the problems, they so far have not fixed them. Late last year, the Government Accountability Office reported that 27 health care providers working in the federal Veterans Affairs system were on the OIG’s exclusion list.
If someone “intentionally omits” from applications they are an “excluded owner or an owner with a felony conviction,” then “there’s no means of immediately identifying the false reporting,” said Dara Corrigan, director of the center for program integrity at CMS. She also said there is “no centralized data source of accurate and comprehensive ownership” to check for violators.
The OIG exclusion list website, which health care companies are encouraged to check for offenders, notes that the list does not include altered names and encourages those checking it to vet other forms of identification.
Gaps in reporting also mean many who are barred may not know they could be violating their ban because exclusion letters can go out months after convictions or settlements and may never reach a person who is in jail or has moved, experts said. The exclusion applies to federal programs, so a person could work in health care by accepting only patients who pay cash or have private insurance. In its review, KHN found some on the exclusion list who were working in health care businesses that don’t appear to take taxpayer money.
OIG said its exclusions are “based largely on referrals” from the Justice Department, state Medicaid fraud-control units, and state licensing boards. A lack of coordination among state and federal agencies was evident in exclusions KHN reviewed, including cases where years elapsed between the convictions for health care fraud, elder abuse, or other health-related felonies in state courts and the offenders’ names appearing on the federal list.
ProviderTrust, a health care compliance group, found that the lag time between state Medicaid fraud findings and when exclusions appeared on the federal list averaged more than 360 days and that some cases were never sent to federal officials at all.
The NPI, or National Provider Identifier record, is another potential enforcement tool. Doctors, nurses, other practitioners, and health businesses register for NPI numbers to file claims to insurers and others. KHN found that NPI numbers are not revoked after a person or business appears on the list.
The NPI should be “essentially wiped clean” when the person is excluded, precluding them from submitting a bill, said John Kelly, a former assistant chief for health care fraud at the Department of Justice who is now a partner for the law firm Barnes & Thornburg.
Corrigan said the agency didn’t have the authority to deactivate or deny NPIs if someone were excluded.
The Family ‘Fronts’
Repeat violators are all too common, according to state and federal officials. KHN’s review of cases identified seven of them, noted by officials in press releases or in court records. KHN also found six who transferred control of a business to a family or household member.
One common maneuver to avoid detection is to use the names of “family members or close associates as ‘fronts’ to create new sham” businesses, said Lori Swanson, who served as Minnesota attorney general from 2007 to 2019.
Blank said the OIG can exclude business entities, which would prevent transfers to a person’s spouse or family members, but it rarely does so.
Thurlee Belfrey stayed in the home care business in Minnesota after his 2004 exclusion for state Medicaid fraud. His wife, Lanore, a former winner of the Miss Minnesota USA title, created a home care company named Model Health Care and “did not disclose” Thurlee’s involvement, according to his 2017 plea agreement.
“For more than a decade” Belfrey, his wife, and his twin brother, Roylee, made “millions in illicit profits by cheating government health care programs that were funded by honest taxpayers and intended for the needy,” according to the Justice Department. The brothers spent the money on a Caribbean cruise, high-end housing, and attempts to develop a reality TV show based on their lives, the DOJ said.
Federal investigators deemed more than $18 million in claims Model Health Care had received were fraudulent because of Thurlee’s involvement. Meanwhile, Roylee operated several other health care businesses. Between 2007 and 2013, the brothers deducted and collected millions from their employees’ wages that they were supposed to pay in taxes to the IRS, the Justice Department said.
Thurlee, Lanore, and Roylee Belfrey all were convicted and served prison time. When reached for comment, the brothers said the government’s facts were inaccurate and they looked forward to telling their own story in a book. Roylee said he “did not steal people’s tax money to live a lavish lifestyle; it just didn’t happen.” Thurlee said he “never would have done anything deliberately to violate the exclusion and jeopardize my wife.” Lanore Belfrey could not be reached for comment.
Melchor Martinez settled with the government after he was accused by the Department of Justice of violating his exclusion and for a second time committing health care fraud by enlisting his wife, Melissa Chlebowski, in their Pennsylvania and North Carolina community mental health centers.
Previously, Martinez was convicted of Medicaid fraud in 2000 and was excluded from all federally funded health programs, according to DOJ.
Later, Chlebowski failed to disclose on Medicaid and Medicare enrollment applications that her husband was managing the clinics, according to allegations by the Justice Department.
Their Pennsylvania clinics were the largest providers of mental health services to Medicaid patients in their respective regions. They also had generated $75 million in combined Medicaid and Medicare payments from 2009 through 2012, according to the Justice Department. Officials accused the couple of employing people without credentials to be mental health therapists and the clinics of billing for shortened appointments for children, according to the DOJ.
They agreed, without admitting liability, to pay $3 million and to be excluded — a second time, for Martinez — according to court filings in the settlement with the government. They did not respond to KHN’s attempts to obtain comment.
‘Didn’t Check Anything’
In its review of cases, KHN found nine felons or people with fraud convictions who then had access to federal health care money before being excluded for alleged or confirmed wrongdoing.
But because of the way the law is written, Blank said, only certain types of felonies disqualify people from accessing federal health care money — and the system relies on felons to self-report.
According to the DOJ court filing, Frank Bianco concealed his ownership in Anointed Medical Supplies, which submitted about $1.4 million in fraudulent claims between September 2019 and October 2020.
Bianco, who opened the durable medical equipment company in South Florida, said in an interview with KHN that he did not put his name on a Medicare application for claims reimbursement because of his multiple prior felonies related to narcotics.
And as far as he knows, Bianco told KHN, the federal regulators “didn’t check anything.” Bianco’s ownership was discovered because one of his company’s contractors was under federal investigation, he said.
Kenneth Nash had been convicted of fraud before he operated his Michigan home health agency and submitted fraudulent claims for services totaling more than $750,000, according to the Justice Department. He was sentenced to more than five years in prison last year, according to the DOJ.
Attempts to reach Nash were unsuccessful.
“When investigators executed search warrants in June 2018, they shut down the operation and seized two Mercedes, one Land Rover, one Jaguar, one Aston Martin, and a $60,000 motor home — all purchased with fraud proceeds,” according to a court filing in his sentencing.
“What is readily apparent from this evidence is that Nash, a fraudster with ten prior state fraud convictions and one prior federal felony bank fraud conviction, got into health care to cheat the government, steal from the Medicare system, and lavishly spend on himself,” the filing said.
As Kelly, the former assistant chief for health care fraud at the Justice Department, put it: “Someone who’s interested in cheating the system is not going to do the right thing.”
KHN Colorado correspondent Rae Ellen Bichell contributed to this report.

